Pharmacometric modelling and simulation: a tool in therapeutic decision-making
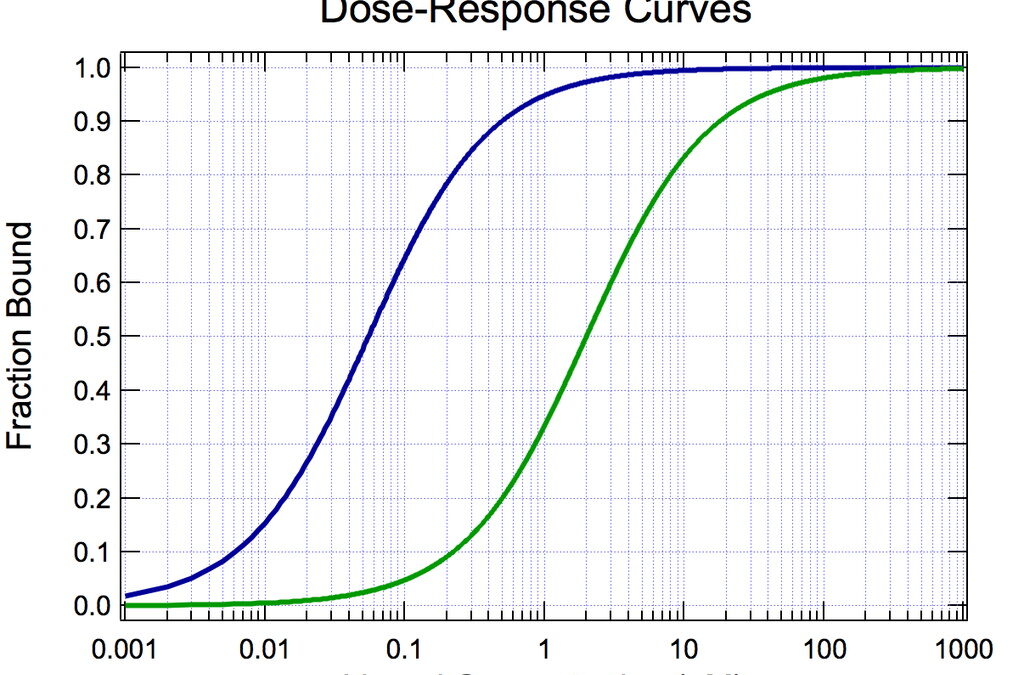
When a medicine is prescribed, a fundamental requirement is to understand very well the dose-response relationship in order to determine how much and how frequently to administer a given treatment. It is important to consider the dosing in both clinical practice and research, which requires a good understanding of pharmacokinetics (PK) and pharmacodynamics (PD).
Pharmacometrics encompasses the analysis of PK and PD data, and then uses resulting models to make inferences (often using simulations) on the optimum dosing for clinical trials practice. An understanding of pharmacometric modelling and simulation, and how it can give insights into the dose-concentration-effect relationship, will be very useful to all clinical pharmacists and pharmacologists.
.
Manju Bhaskar, PhD, CRP, Consultant
Clinical Research Academy Montreal
.
The term modelling refers to mathematical and statistical modelling. A mathematical model is defined as an equation used to relate known covariates (dose given, time of dose, time of observations) with observed measurements. All the models are gross simplifications of the system under study, and so the goal of PK/PD modelling is often to test a range of models to determine which fits best. Clinical pharmacologists tend to choose specific models using a knowledge of the system that generated the observed data.
In the early 2000s, this science gained impetus when pharmacometric analyses started to influence the drug development decisions and regulatory approvals. Another turning point was the introduction of clinical trial simulations, or Computer Assisted Trial Design (CATD) methodologies as tools to use phase I and phase II exposure-response information for the design phase III trials, predict the trial outcomes in terms of efficacy and safety, and allow for more informational decisions on the benefit/risk analysis and the economics of drug development programs.
Pharmacometrics influenced high-level decisions such as the trial design, drug approval and labeling. The clinical trial simulation of the Cellcept (mycophenolate mofetil) in renal transplants is a classic example of model-based trial design. Drugs, such as the Toradol (analgesic), the Remifentanil (analgesic), Netrecor (treatment of congestive heart failure), Neurontin (treatment of post-herpectic neuralgia) were also approved by modelling and simulation.
Clinical trials being the most consistently progressing area of research, devising strategies to utilize pharmacometrics as an analytical tool to its fullest potential is the need of the hour. Pharmacometricians can develop the tools to implement several fundamental PK, clinical pharmacology, and statistical concepts, and impart advanced technical training to budding candidates.
A comprehensive learning of the essential components, such as disease areas and drug development principles, is essential to enhance the therapeutic decision-making abilities in the clinical setting. Development of a more integrated software is critical to industrialize pharmacometric projects. Another important aspect is sharing the success stories how a pharmacometric-based solution is a critical step in therapeutic decision-making. The future of pharmacometrics depends on how the industry, regulatory agencies, and academia can thrive together to strategize these goals.
Bibliography
- Lesko LJ and Sahajwalla C. Introduction to Drug Development and Regulatory Decision-Making. New Drug Development, Marcel Dekker Inc. 2004, Vol 141, pp. 1-14.
- Gieschke R and Steimer JL. Pharmacometrics: modelling and simulation tools to improve therapeutic decision making in clinical drug development, 2000, Vol 25, no.1, pp. 49-58.
- Gobburu JVS. Pharmacometrics 2020. Journal of Clinical Pharmacology, 2010; 50:151S-175S.